Abstract
Background: A younger haplo donor is usually preferred over an older donor. However, when several donors of similar ages are available, which factors should be prioritized remains a matter of debate. This is a frequent clinical question for older recipients who are undergoing haplo hematopoietic cell transplantation (HCT) from a child donor. Although conventionally a female donor is avoided for a male recipient due to the high risk of graft-versus-host disease (GVHD), this has not been consistently seen in the setting of T cell-replete haploidentical HCT with post-transplant cyclophosphamide (PTCy) prophylaxis. Additionally, there is increasing recognition of the impact of (mis)matches at specific HLA loci with haplo HCT. Whether HLA factors trump non-HLA factors (e.g female-to-male, donor age, relationship), or vice-a-versa, is unclear. As patient and donor ages and relationships are important predictors of outcomes and are very tightly correlated to each other, we studied the effects of HLA and non-HLA factors stratified by donor relationship (son vs daughter).
Objective: We sought to compare the outcomes of T-cell replete haplo HCT using a son vs daughter donor with PTCy prophylaxis, after accounting for (mis)matching at individual HLA loci and patient/donor age.
Results: We included 298 consecutive patients with a daughter (n=96) vs son (n=202) donor. Median age at HCT (56 yrs vs 58 yrs, p=0.05) and donor age (27 yrs vs 29 yrs, p=0.1) were similar in both groups. Most received RIC (78% vs 76%, p=0.5) and had HCT-CI >3 (52% vs 54%, p=0.6). Fewer patients with a daughter donor received BM graft (56% vs 74%, p=0.002) and had high/very high DRI (20% vs 41%, p<0.001). Most patients were CMV seropositive (83% vs 81%, p=0.09) and ABO matched with donor (60% vs 61%, p=0.9). Significantly more patients with a daughter donor had HLA-C mismatch (97% vs 88%, p=0.01); other mismatches were similar in both groups: A (91% vs 96%, p=0.2), B-leader (43% vs 37%, p=0.6), DRB1 (92% vs 94%, p=0.5), DQB1 (86% vs 90%, p=0.3), DPB1 (76% vs 80%, p=0.4). The median follow-up was 24 vs 27 months.
Graft failure occurred in 2% vs 4%, p=0.5; the median time to neutrophil engraftment was similar (20 vs 19 days). The cumulative incidence of grade II-IV aGVHD (39% vs 34%, p=0.5) and grade III-IV aGVHD at day 180 (12% vs 6%, p=0.1), 2-yr cGVHD (18% vs 12%, p=0.4); NRM (28% vs 33%, p=0.5), relapse (24% vs 29%, p=0.4), PFS (47% vs 38%, p=0.2) and OS (50% vs 46%, p=0.4) were similar in daughter vs son, respectively.
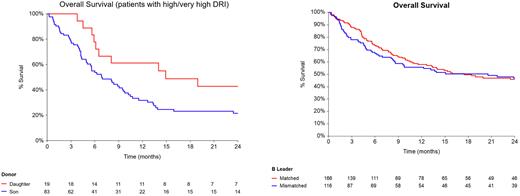
In multivariate analysis, daughter donors were associated with similar risk of grade II-IV aGVHD (HR 1.2, 95% CI 0.8-1.9, p=0.3), cGVHD (HR 1.03, 95% CI 0.5-2.3, p=0.9), and NRM (HR 0.9, 95% CI 0.6-1.4, p=0.7) as sons. For survival, significant interactions were noted between donor gender and DRI. In patients with low DRI, there was no impact of donor gender, but in patients with high/v high DRI, daughter donors were associated with improved PFS (HR 0.5, 95% CI 0.2-0.9, p=0.03) and OS (HR 0.5, 95% CI 0.3-0.9 p=0.04) as compared to sons. Relapse rate was highest with son-to-mother (HR 1.7, 95% CI 1.02-2.7, p=0.04).
PB graft was associated with a significantly higher risk of cGVHD (HR 3.1, 95% CI 1.5-6.4, p=0.003). High/very high DRI was associated with a high risk of relapse (HR 2.4, 95% CI 1.5-3.9, p<0.001). Patient age >50 yrs had high NRM (HR 2.03, 95% CI 1.1-3.7, p=0.02), poor PFS (HR 1.5, 95% CI 1.02-2.3, p=0.04) and OS (HR 1.6, 95% CI 1-2.5, p=0.05). There was no significant impact of specific HLA mismatches on any of the outcomes. Having 3 class II HLA (vs <3) mismatches was associated with a high risk of cGVHD (HR 3.3, 95% CI 1.3-8.7, p=0.01), with no impact on survival.
Conclusion: Among child haplo donors, our data suggest that female donors do not result in any inferior outcomes as compared to male donors. A daughter may even be a preferred donor for patients with high/very-high DRI as it conferred survival benefit as compared to a son donor. This may partly be related to a higher risk of relapse seen in son donor to mother recipient. Also, certain HLA mismatches (e.g. B-leader), which have prognostic implications in haplo HCT in general, did not appear to be of significance when accounted for donor relationship and age in patients with a child donor. Further large-scale studies are needed to comprehend these complex immunobiological relationships.
Disclosures
Mehta:Syndax: Research Funding; Orca Bio: Research Funding. Alousi:Prolacta: Consultancy; Genetech: Consultancy; Sanofi / Kadmon: Honoraria; Mallinkrodt: Honoraria; Incyte: Honoraria, Research Funding. Kebriaei:Jazz: Consultancy; Kite: Consultancy; Amgen: Research Funding; Pfizer: Consultancy; Ziopharm: Research Funding. Nieto:Secura Bio: Research Funding; Affimed: Other: Scientific advisory Board, Research Funding; Astra Zeneca: Research Funding. Oran:AROG: Research Funding; ASTEX: Research Funding. Popat:Bayer: Research Funding; Incyte: Research Funding; Abbvie: Research Funding; Novartis: Research Funding; Iovance: Consultancy. Srour:Orca Bio: Research Funding. Rezvani:GemoAb: Other: Participates on the Scientific Advisory Board ; AvengeBio: Other: Participates on the Scientific Advisory Board ; Virogin Biotech: Other: Participates on the Scientific Advisory Board ; GSK: Other: Participates on the Scientific Advisory Board ; Bayer: Other: Participates on the Scientific Advisory Board ; Navan Technologies: Other: Participates on the Scientific Advisory Board ; Caribou Biosciences: Other: Participates on the Scientific Advisory Board ; Takeda: Patents & Royalties, Research Funding; Affimed: Research Funding. Champlin:Johnson &Johnson: Consultancy; General Oncology: Other: Data Safety Monitoring Board; Bluebird: Other: Data Safety Monitoring Board; Cell Source Inc.: Research Funding; Omeros: Consultancy; Actinium: Consultancy; Kadmon: Consultancy. Shpall:Bayer: Honoraria; Affimed: Other: License agreement; Takeda: Patents & Royalties; Fibroblasts and FibroBiologics: Consultancy; Navan: Consultancy; adaptimmune: Consultancy; NY blood center: Consultancy; axio: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal